Coronavirus disease-2019 in the autopsy room
Dr Emyr W Benbow
Honorary Consultant Pathologist, Manchester Royal Infirmary
By March 20th 2020, officially the First Day of Spring, 108 deaths had been recorded by the Office of National Statistics, of individuals confirmed to have died of Coronavirus Disease-2019 (CoVid-19). Remember those heady days, when we smugly thought HM Government must have something seriously smart up their collective sleeve, otherwise they would have been galvanised into some sort of effective action? And then we gradually realised that the sleeve was empty of the rabbit we expected them to pull out of the hat (oops, I’ve mixed my metaphors there, but then, these are very strange times indeed). After all, we'd already heard how they would follow the science; we simply hadn't realised that they would indeed follow the science, but about three weeks too late. As we now know, that period has have proved to be crucial, and many have lost the rest of their potential lives, for the sake of those three weeks of bluster and dither. The half-truths have continued to flow, and no-one has managed to explain to Boris that two half-truths do not add up to a whole truth.
On March 23rd our team of autopsy pathologists met, in a room carefully selected to allow appropriate social distancing, to discuss how we would proceed. The unanimous decision was that we would continue with our autopsy service, but that we would be very insistent about appropriate measures to ensure our safety: we had very rapidly surmised that this virus’ incubation period was variable, and noted the fact that many of those infected have few or no symptoms. Our usual risk assessment procedure is to determine if there is a recognised danger, for each individual case, of blood-borne or airborne infection. This procedure has now been largely set aside, and we now regard every autopsy as carrying a significant risk of airborne infection. Of course, we are also very aware that risk factors for blood-borne infection do not protect from CoViD-19, so we still look for blood-borne risk factors, too. And wear that extra glove or two.
We were already aware that CoViD-19 was due to a virus in Hazard Category 3, but that we would be allowed to perform laboratory work in conditions appropriate for Hazard Category 2 organisms – view here (section 5). You’ll remember the publicity about keeping the NHS safe, and I naively thought that this was to do with capacity for intensive care beds; at this point, we were all far from realising that this was just stalling because the real limitation was the personal protective equipment that the nation had in store – or, rather, its lack. After all, where national austerity has been the driving force over much of the last decade, why would you keep up the stocks of PPE, when you just can stick you head in the sand and hope the inevitable pandemic won’t appear on your watch? The only tiny surprise is that it was not the predicted influenza outbreak (Anonymous. World Is Ill-Prepared for "Inevitable" Flu Pandemic. Bull World Health Organ. 2004 Apr; 82 (4): 317-8). 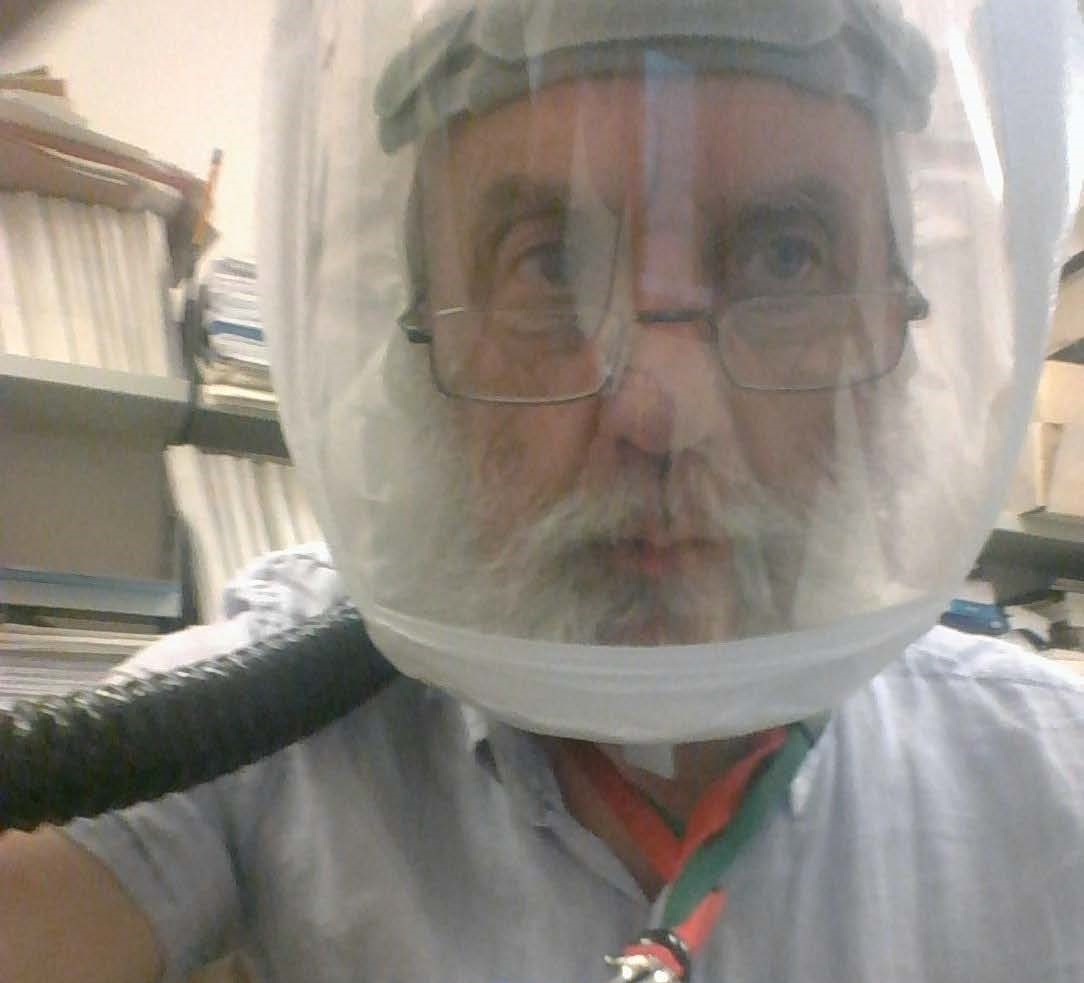
I’ve found it satisfying to realise I can still learn, despite having a head already overfull of assorted rubbish. Sadly, it has taken the presence of a virus leading to the deaths of many thousands to enable me to realise that I can learn new things about new diseases, and new ways of communicating about those new diseases. I have learned the features of a disease only discovered as a new entity a few weeks earlier ago, and to have the confidence to make a diagnosis of CoViD-19 on the basis of autopsy and histology alone, at least with the degree of confidence required by the Coroner: of course, all that evidence of acute lung injury, with little or no bronchopneumonic change, could be a lot of other things. Of course, it helps when the clinical records have stated, over and over again, that despite the negative swabs, the intensivists have deliberately continued to treat as CoViD-19, usually with radiological support. The Coroner wants diagnoses to satisfy the criterion of the balance of probabilities, and that’s when the epidemiological background is worth understanding: currently, about half the excess deaths compared to last year have not been shown to be positive on PCR, so do we assume there a second epidemic with a different agent? Of course we don’t, even though a few are natural deaths in people who have chosen to avoid hospitals, or suicides in those lacking support, or scared of the whole bewildering situation. Taking the epidemiological background into account, I think that that pattern of acute lung injury puts the diagnosis of CoViD-19 close to beyond the reasonable doubt required of criminal law. And that is ironic, given the failings of those in charge of the nation.
What makes me secure in my understanding of CoViD-19, and what it looks like? A lot of this experience is based on patients diagnosed with CoViD by swabs in life (and I understand that false positives swabs are far less likely than false negatives), but where autopsy investigation was required because they were post-operative deaths, deaths from alleged industrial lung disease, and so on. Others were patients who had died in the community, and where the clinical history had nothing to suggest CoViD (for example, because the subject had lived and died alone) but I took the swabs anyway. Let me add that this wasn’t wanton waste of precious swabs: this was targeted because I’ve learned that there is a very striking appearance of the mucosa in the trachea and major airways that is strongly predictive of a positive swab, or of CoViD-typical microscopic changes in the more peripheral lung tissue, or both. I have nothing other than anecdotal evidence and gut feeling (and mainly the latter) to support my strategy, but I swab the nasopharynx in the usual way, and then the mucosa just below the tracheal bifurcation after carefully opening down the membranous portion. And put both swabs in the same vial of transport medium, so it takes just one PCR run, not two.
Pathologists have repeatedly preached that the autopsy is worth preserving because it helps us understand disease and thus to save future lives. I did a lot of this preaching, especially in the aftermath of the Bristol and Alder Hay scandals, so any course other than the one I’ve taken was unthinkable. However, I'm no fool, and I realise that I’m rapidly approaching at least one risk factor for an adverse outcome to viral infection, that of a serious degree of antiquity. By the time of that first meeting, and the discussion of personal protection equipment, I had already contemplated becoming clean shaven for the first time in over 50 years. This wasn’t anything to do with the autopsy service: it arose because one of my friends and colleagues in the medical school hierarchy knew I’d considered myself as pretty slick at taking blood and inserting cannulae whilst a house officer – and when that friend (he’s an intensivist) took on a very senior role in the “CoViD Hospital”, he offered me a crash course of re-training. I hesitated because policies seemed to emerge and change on a daily basis - and never failing a cannulation in 1978 doesn’t guarantee success in 2020. And the pressure on the ward didn’t ever get so that desperate that I was ever asked to help.
When we discussed PPE for the autopsy service, I knew the Department is well supplied with powered respirators and Jupiter masks, which easily enclose my entire face. So my beard (older than many of our politicians, and wiser than perhaps all of them) remains. As you can see in Figure 1, the Jupiter mask headgear not only fits around the hair on my face, but also the rapidly diminishing hair on my head, so we have a win-win situation. Modern Jupiter masks have become lighter than older models, and are surprisingly comfortable and easy to wear - though the weight of the motor and powerpack on your lower back can become marginally annoying after four or five hours in the autopsy room. I really like that moment when I switch the device on, and the mask bulges out from under my chin because of the positive air pressure: it is an extremely satisfying and comforting sensation, to realise that this thing is actively blowing droplets and aerosols away from my face.
The histological appearance of CoViD-19 resembles diffuse alveolar damage (or adult respiratory distress syndrome, for any clinical reader), but in my experience, the hyaline membranes are much more patchy, even in patients who have survived prolonged ventilation before eventually succumbing. This reflects the naked eye features, which are also far short of the changes noted in full-blown “ITU lung”. Granted, CoViD lungs are congested and blotchy, but they lack the diffuse firmness that otherwise characterises the diffuse alveolar damage that used to follow prolonged but ultimately unsuccessful ventilation. The findings in the major airways are also helpful, even in patients with a history of chronic obstructive airways disease . You may have to gently remove the mucopurulent plugs of an acute COAD exacerbation, but beneath it, the CoViD mucosa has a soft pink mushy appearance that I find strongly predictive of a positive swab, or of typical CoViD histology. There are also other features which help, and a number of publications have indicated the presence of a typical multinucleate cell, generally small, and filled with regularly spaced nuclei. I've also been impressed by the presence of a very subtle pericarditis, characterised macroscopically by a stickiness between the pericardial layers, and microscopically by slightly enlarged lymphocytes or plasmacytoid cells, sometimes extending throughout the myocardium.
Early on in the pandemic, we were told that swabs should not be wasted on people already dead. I'm very proud to have friends in the Department of Virology, who agreed with my view that we needed to know what was going on in those dying in the community, a view strongly supported by the more recent epidemiological evidence that the numbers of excess deaths are somewhere close to twice those recorded as due to CoViD-19. Some of these, of course, will be because of the fact that the health services are distracted by CoViD-19, and patients with chronic diseases will have identified that hospitals are dangerous for them, only to succumb to those diseases in their homes. We must also be aware that people are dying in the community with CoViD-19, typically in combination with other chronic diseases, but their Death Certificates will only show those pre-existing chronic diseases.
I was asked by your Editor to provide photomicrographs, but I can’t: some months ago, my desktop computer was upgraded to accommodate Microsoft Windows 10 Enterprise, and our local IT team have since worked very hard to restore all sorts of important functions wrecked by that upgrade. They’ve done very well, but the software for my camera system remains defunct. Ironically, a team from the microscope manufacturer was expected to visit – on the day that became the first day of lockdown. They never arrived, and I assume they are still working from home. One of my colleagues has, very kindly indeed, taken a few photographs of a degenerate myocardial cell that appears in the myocardium of some cases, but I can’t ask for a comprehensive set of images: it wouldn’t be fair to take that much of his time, and it wouldn’t be fair to breathe on his microscope while I took them myself.
Finally, CoViD-19 has enabled me to learn a skill which I never even knew I might need – that of preparing for and participating in a live webinar: follow this link below, and ignore the first, floundering speaker. There’s a lot to learn about staying safe in laboratories in the CoViD-19 era – an era that, if we’re unlucky and those promising vaccines don’t live up to their promises, could be the rest of your working lives.
View webinar
And finally, again: does anyone else find the name of this disease sinister? Why call it coronavirus disease-2019 if you aren’t anticipating coronavirus disease-2020? And its many little cousins? I’m off to polish my Jupiter mask.
These opinions are entirely those of the author, and possibly no-one else: they do not represent the official view of the BDIAP, the University of Manchester or Manchester University NHS Trust.