At the start of the COVID-19 pandemic in Spring last year, the scientific community did not understand the disease nor the full extent of its manifestations. Histopathology as a gold standard, especially through the undertaking of autopsies, helped us to understand the effects of the virally induced changes and contributed to research through investigations into disease biology through to improving patient management.
Please find below 3 different perspectives from different centres and their approach to COVID-19 autopsies.
COVID-19 Autopsies
Vivek Sekhawat & Sebastian Lucas
 The ongoing global COVID-19 pandemic has brought into the spotlight the critical role and necessity of autopsy. The rapid spread of infection has resulted in overload of healthcare services internationally, and the medical community continues to face difficulties in developing effective treatments for a disease pathophysiology that is incompletely understood. Several factors have impacted the ability of pathologists to respond to this need. Understandable concerns for safety and limiting the spread of infection, particularly early on in the crisis when transmission was less fully understood, have meant that fewer autopsies could be justifiably performed, within both the Coronial and hospital settings in the UK. In addition, the burdens on healthcare services have imposed significant resource limitations. Mortuary services have been under tremendous strain in managing the flow of bodies, and clinical teams have worked in trying conditions with restrictions placed on visiting relatives, which has affected communications and the ability to acquire consent for autopsies.
The ongoing global COVID-19 pandemic has brought into the spotlight the critical role and necessity of autopsy. The rapid spread of infection has resulted in overload of healthcare services internationally, and the medical community continues to face difficulties in developing effective treatments for a disease pathophysiology that is incompletely understood. Several factors have impacted the ability of pathologists to respond to this need. Understandable concerns for safety and limiting the spread of infection, particularly early on in the crisis when transmission was less fully understood, have meant that fewer autopsies could be justifiably performed, within both the Coronial and hospital settings in the UK. In addition, the burdens on healthcare services have imposed significant resource limitations. Mortuary services have been under tremendous strain in managing the flow of bodies, and clinical teams have worked in trying conditions with restrictions placed on visiting relatives, which has affected communications and the ability to acquire consent for autopsies.
Read full article.
Coronavirus disease-2019 in the autopsy room
Emyr W Benbow
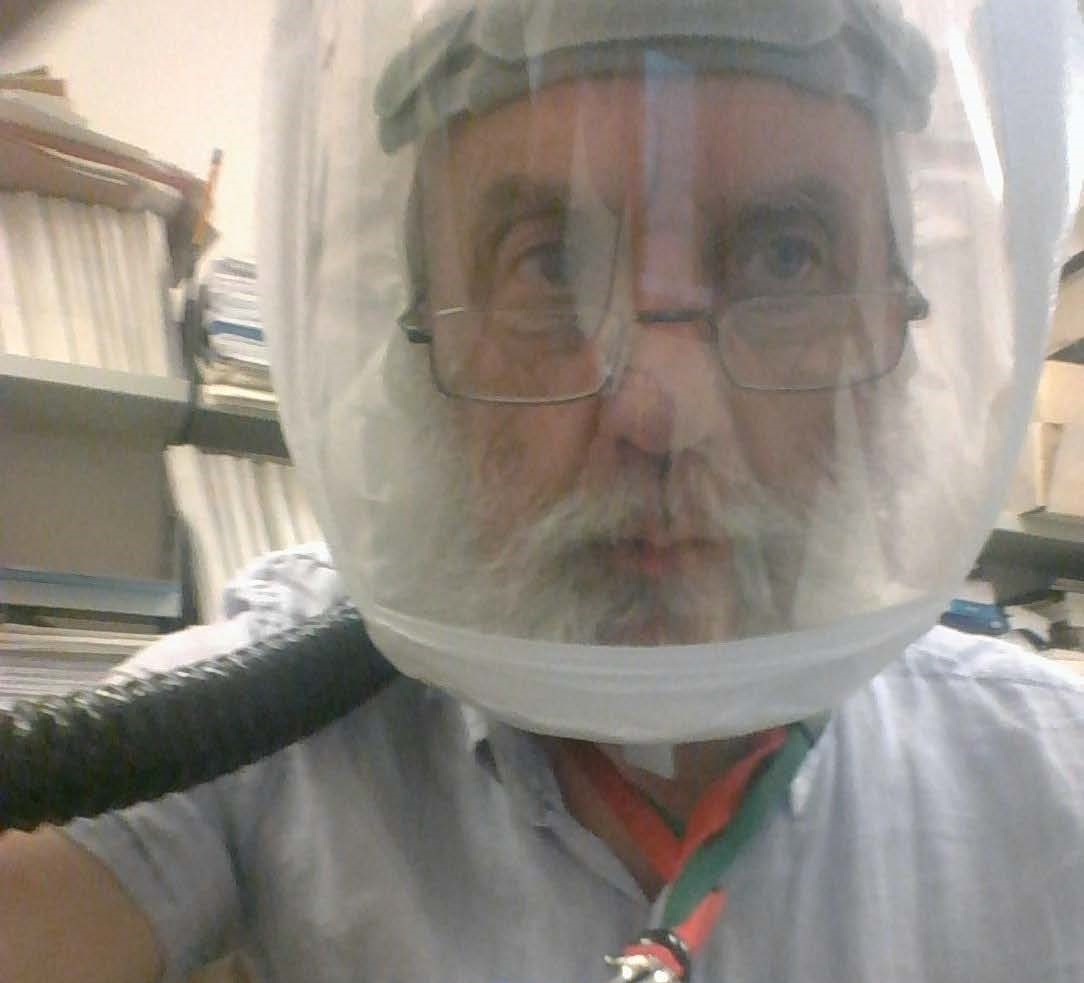 By March 20th 2020, officially the First Day of Spring, 108 deaths had been recorded by the Office of National Statistics, of individuals confirmed to have died of Coronavirus Disease-2019 (CoVid-19). Remember those heady days, when we smugly thought HM Government must have something seriously smart up their collective sleeve, otherwise they would have been galvanised into some sort of effective action? And then we gradually realised that the sleeve was empty of the rabbit we expected them to pull out of the hat (oops, I’ve mixed my metaphors there, but then, these are very strange times indeed). After all, we'd already heard how they would follow the science; we simply hadn't realised that they would indeed follow the science, but about three weeks too late. As we now know, that period has have proved to be crucial, and many have lost the rest of their potential lives, for the sake of those three weeks of bluster and dither. The half-truths have continued to flow, and no-one has managed to explain to Boris that two half-truths do not add up to a whole truth.
By March 20th 2020, officially the First Day of Spring, 108 deaths had been recorded by the Office of National Statistics, of individuals confirmed to have died of Coronavirus Disease-2019 (CoVid-19). Remember those heady days, when we smugly thought HM Government must have something seriously smart up their collective sleeve, otherwise they would have been galvanised into some sort of effective action? And then we gradually realised that the sleeve was empty of the rabbit we expected them to pull out of the hat (oops, I’ve mixed my metaphors there, but then, these are very strange times indeed). After all, we'd already heard how they would follow the science; we simply hadn't realised that they would indeed follow the science, but about three weeks too late. As we now know, that period has have proved to be crucial, and many have lost the rest of their potential lives, for the sake of those three weeks of bluster and dither. The half-truths have continued to flow, and no-one has managed to explain to Boris that two half-truths do not add up to a whole truth.
Read full article (includes a link to a webinar).
Post mortem practice during a pandemic: identifying the indirect casualties of COVID 19
Robert Pell and Ian Roberts
Regular readers of the BDIAP newsletter will probably agree that the elective placement opportunities provided by the society are one of the key highlights. Unfortunately my tale of interesting experience involved volunteering for redeployment to acute medicine at the John Radcliffe Hospital, Oxford. I had previously trained in medicine (obtaining my MRCP in 2010) and so ventured back to clinical practice for (hopefully) one last time. 
It became clear early on during the epidemic that COVID 19 incorporated a variety of clinical presentations that were not just restricted to fever, cough and dyspnoea. We were required to update ourselves on the clinical manifestations of this disease on an almost daily basis, and rapid dissemination of current practice occurred at an unprecedented rate. Although electronic resources were and continue to be a key resource in disseminating information widely and rapidly, traditional clinician to clinician contact was often the first way we discovered new disease manifestations. One example was a colleague forwarding a diabetes UK circular on COVID 19 presenting as newly diagnosed diabetic ketoacidosis published the day before we admitted our first case. Appreciation of the dramatic rise in mortality in patients with decompensated cirrhosis and COVID 19 came from bumping into a hepatology registrar on a ward round. Late skin manifestations (‘COVID toes’) were learnt from a conversation in the doctor’s mess. I was able to feed this clinical insight back to the department to help the service adapt during the epidemic: pathology certainly was not left behind!
Read full article.
Further articles from trainees
Histopathology trainees share their experiences of COVID-19. View the articles here.